Sickle cell disease dispropportionately affects Black people and increase risk of COVID-19
Patients with sickle cell disease may be at higher risk for certain COVID-19 complications and death, according to results of two studies presented at ASH Annual Meeting and Exposition.
Patients with sickle cell disease may be at higher risk for certain COVID-19 complications and death, according to results of two studies presented at ASH Annual Meeting and Exposition.
In one study, Lana Mucalo, MD, postdoctoral fellow at Medical College of Wisconsin, and colleagues found that individuals with sickle cell disease faced 6.2 times the risk for COVID-19-related mortality compared with the general Black population.
There are several possible explanations for this finding, Mucalo told Healio.
“Patients with sickle cell disease are more likely to have a high prevalence of the various comorbidities that can put individuals at high risk [for] severe illness and death,” she said. “Also, previous studies show that [patients with sickle cell disease] have worse outcomes due to influenza infection compared with the general population, so respiratory viral infections, potentially COVID-19 too, are a significant source of morbidity and mortality for them.”
In another study, Ashima Singh, MS, PhD, research scientist in the department of pediatrics at Medical College of Wisconsin, and colleagues found that patients with sickle cell disease and COVID-19 may be more at risk for hospitalization, pneumonia and pain than Black individuals with COVID-19 but without sickle cell disease, although their study did not demonstrate and increased risk for mortality.
Patients with preexisting conditions are known to have poorer outcomes from COVID-19, but whether that also applied to patients with sickle cell disease — which occurs primarily among Black individuals — had been unknown.
Also, COVID-19 has been shown to disproportionately impact Blacks, with a 22.2% death rate among Black patients compared with a 13% death rate for the general population, according to the researchers.
“There is really very limited knowledge of COVID-19 outcomes among individuals with sickle cell trait,” Singh told Healio.
Higher case fatality, hospitalization rates
In the first study, Mucalo and colleagues used data from the international SECURE-SCD Registry — a voluntary reporting system developed at Medical College of Wisconsin to collect data on children and adults with COVID-19 and sickle cell disease — to compare COVID-19 hospitalization and case fatality rates among those with sickle cell disease in different age groups with the general Black population. For the latter group, researchers used data from the California Department of Public Health for case fatality rates and from COVID-NET for hospitalization rates.
Researchers also evaluated factors associated with more severe COVID-19 illness and hospitalization among those with sickle cell disease.
“The goal was to collaboratively capture real-time data at one place and identify risk factors and their impact on health outcome,” Mucalo told Healio.
The analysis included 152 children (mean age, 10.9 years; 46.7% female) and 214 adults (mean age, 34 years; 58.1% women) with sickle cell disease and COVID-19, most of whom (n = 324) were from the U.S.
Researchers reported hospitalization rates of 46.1% among children and 66.8% among adults, and death rates of 0.7% among children and 7% among adults.
The COVID-19 case fatality rate was higher among those with sickle cell disease than among Black individuals in the general California population for all age groups, including ages 0 to 17 years (0.8% vs. 0%), 18 to 34 years (2.6% vs. 0.4%), 35 to 49 years (11.9% vs. 1%), 50 to 64 years (17.6% vs. 3.8%) and 65 to 79 years (20% vs. 15%). The case fatality rate was highest in the general population among those aged 80 years or older, at 34.3%, but there were no patients in the sickle cell disease cohort in this age group for comparison.
Overall, these data showed patients with sickle cell disease were 6.2 times more likely to die of COVID-19 infection, according to Mucalo.
Children with sickle cell disease had higher hospitalization rates than those in the general population in the age groups of 0 to 4 years (4.2% vs. 0.6%) and 5 to 17 years (26.2% vs. 1%).
Hospitalization rates peaked among those with sickle cell disease in age group of 18 to 49 years, at 59.7%, and at age 65 years and older for the general population, at 37.4%.
Results of a multivariable model shows factors associated with hospitalization among children with sickle cell disease included requiring three or more ED visits/hospitalizations for acute pain events within the prior 3 years (OR = 4.64; 95% CI, 1.97-10.9); heart and lung manifestations of sickle cell disease, such as pulmonary hypertension or acute chest syndrome (OR = 4.17; 95% CI, 1.56-11.15); and neurobehavioral disorders, such as stroke, seizure disorder and behavioral problems, among others (OR = 2.73; 95% CI, 1.09-6.81).
Requiring acute care for pain also was associated with a more severe course of COVID-19 among children (OR = 3.96; 95% CI, 1.42-11.06).
Sickle cell disease genotype and use of hydroxyurea did not appear linked to COVID-19 severity or hospitalization. Age was the only risk factor that met significance among adults.
These data may be limited by selection bias, with overrepresentation of patients with more severe illness and underrepresentation of areas with a lack of testing, according to Mucalo. Also, the case fatality rate for the general population was derived from only one state.
“These patients should be following recommended precautions such as mask-wearing, hand hygiene and social distancing,” she told Healio. “It is important that health care providers are aware that [patients with sickle cell disease] are a high-risk group, so they are able to provide proper care in shortest time.”
COVID-19 manifestations
Singh and colleagues conducted a retrospective cohort study using TriNetX — a research network comprised of de-identified patient-level electronic health record data from more than 30 U.S. sites — to compare outcomes of individuals with sickle cell disease and trait with those of Black individuals who did not have sickle cell disease or trait. They hypothesized that those with sickle cell disease would be at risk for poorer COVID-19 outcomes than Black individuals without sickle cell disease/trait, but that those with sickle cell trait alone would not be at higher risk.
The analysis included three patient cohorts: patients with COVID-19 and sickle cell disease (n = 214; mean age, 31.9 years; 63% women), patients with COVID-19 and sickle cell trait (n = 260; mean age, 40.1 years; 81% women), and Black patients with COVID-19 who did not have sickle cell disease or trait (n = 29,992; mean age, 45.8 years; 60% women). Researchers compared these cohorts using 1:1 propensity score matching based on the greedy nearest-neighbor matching algorithm.
The researchers’ outcomes of interest included COVID-19 manifestations, hospitalization and death within 2 weeks of diagnosis.
Results showed higher or similar rates of these outcomes among patients with COVID-19 and sickle cell disease and those with COVID-19 and sickle cell trait, including for cough/fever (disease, 29%; trait, 26%), pain (43%; 19%), dyspnea/shortness of breath/hypoxia (16%; 17%), pneumonia (23%; 13%), acute respiratory distress syndrome/respiratory failure/need for mechanical ventilation (11%; 8%), hospitalization (38%; 15%) and death (5%; 4%).
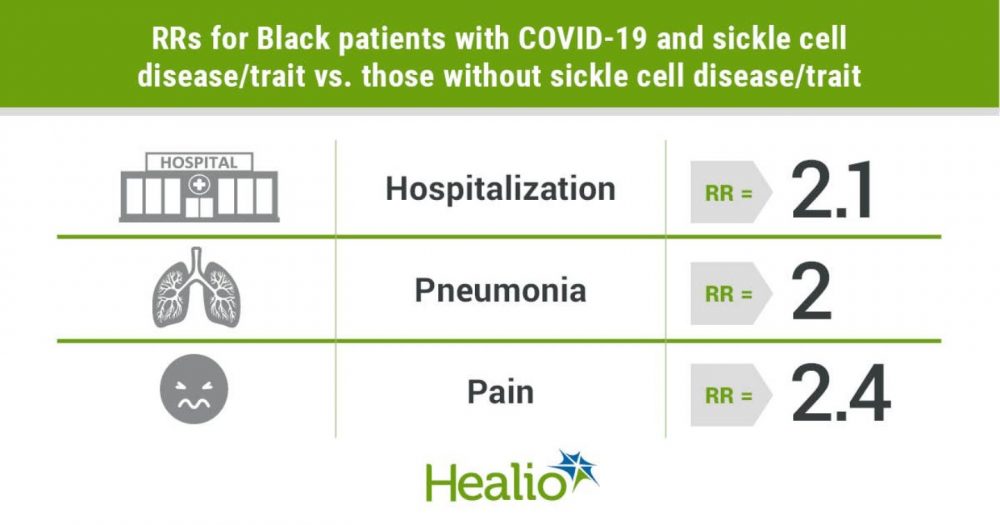
Compared with the group of Black patients with COVID-19 but no sickle cell disease/trait, those with sickle cell disease and trait appeared at significantly greater risk for hospitalization (risk ratio [RR] = 2.1; 95% CI, 1.5-2.9; risk difference, 19.9%; 95% CI, 11.5-28.3), pneumonia (RR = 2; 95% CI, 1.3-3; risk difference, 11.4%; 95% CI, 4.2-18.5) and pain (RR = 2.4; 95% CI, 1.7-3.3; risk difference, 25.1%; 95% CI, 16.6-33.6). However, researchers did not observe a difference in risk for mortality or other COVID-19 manifestations between these two groups.
Patients with sickle cell trait and COVID-19 did not demonstrate any significantly increased risks for the outcomes measured compared with those without sickle cell disease/trait.
“Based on these data, we conclude that patients with sickle cell disease are almost two times more likely to be hospitalized and to develop pneumonia and pain due to COVID-19 than Blacks who do not have sickle cell disease/trait,” Singh said during her presentation. “But, we found no significant differences in COVID-19 outcomes between individuals with sickle cell trait and Blacks who do not have sickle cell disease/trait.”
A difference in the comparison group between this study and that of Mucalo and colleagues may explain the differences related to the risk for mortality, Singh told Healio.
“In our study, we matched patients on age, gender and other preexisting comorbidities and compared outcomes; so, the comparison group is not exactly the general population and has higher prevalence of comorbidities than the general population,” she said. “Whereas, Dr. Mucalo’s study compared the mortality rate for patients with sickle cell disease with the general population and does not adjust for other preexisting comorbidities.”
Future studies are needed to determine the long-term effects of COVID-19, Singh added.
“Also, the main limitation of our study is that it is based on EHR administrative data, and sickle cell trait is often underdiagnosed,” she said. “More studies are needed to determine COVID-19 outcomes for the sickle cell trait population.”
References:
- Mucalo L, et al. Abstract 16. Presented at: ASH Annual Meeting and Exposition (virtual meeting); Dec. 5-8, 2020.
- Singh A, et al. Abstract 302. Presented at: ASH Annual Meeting and Exposition (virtual meeting); Dec. 5-8, 2020.

